Radiology services are a critical part of New Zealand’s public healthcare system, providing essential diagnostic services to patients.
But APEX is alarmed that Te Whatu Ora / Health New Zealand’s public radiology services have never been under such sustained pressure. This report details how radiology services are unravelling from the perspective of those who work in the system.
You can read the report in full on this page, or download a pdf copy here:
Inside the Unravelling of Public Radiology and Medical Imaging
Introduction
What are radiology services
Radiology can best be thought of as the “eyes of modern medicine”, the branch of healthcare which through medical imaging provides doctors and other health professionals with the ability to see inside the body.
These images are produced by medical imaging technologists operating specialist equipment. Medical Imaging Technologists (MITs), also known as radiographers, are the essential health workforce responsible for producing medical imaging. Sonographers are the primary health workforce who performs ultrasound scans.
The images produced are then read and reported on by radiologists, medical doctors trained in interpreting medical images. Medical imaging and the reports on them, are then used directly by medical professionals such as physicians, surgeons and general practitioners to diagnose and treat a wide variety of health conditions, from strokes and cancers to broken and fractured bones.
APEX is a union of allied, scientific and technical health professionals and represents over 1500 MITs, and 350 sonographers, including those working in
Te Whatu Ora, and in private radiology services. This report focuses primarily on radiology services delivered by medical imaging technologists.
How and why we produced this report
In early 2025 we began hearing reports from MITs of radiology services under extensive pressure, including in Taranaki, Wellington and Auckland. We also started hearing from employees in radiology services worried about the overall state and direction of their district’s radiology services, as the Te Whatu Ora hiring freeze and the repeated refusal of senior leaders to fund needed expansions of radiology services contributed to push some services to the point of collapse. At the same time, we became aware that private radiology services were aggressively expanding, hiring staff and setting up new radiology sites, potentially seeking to pick up outsourcing contracts from Te Whatu Ora.
Concerned to understand the full extent of these dynamics within Te Whatu Ora’s public radiology services, we began work on this report, with a view to understanding the overall state of radiology and setting out some recommendations on a recovery plan for radiology services.
In June and July 2025, APEX surveyed 1200 members working as MITs and received 443 responses. Responses were received from members working in the 20 districts of Te Whatu Ora including Northland, Auckland, Counties Manukau, Waitematā, Waikato, Bay of Plenty, Lakes, Taranaki, Tairāwhiti Hawke’s Bay, Midcentral, Whanganui, Wairarapa, Hutt, Capital and Coast, Nelson Marlborough, Canterbury, South Canterbury, West Coast and Southern.
Respondents reported working across a range of imaging modalities, with the majority working in X-Ray (78.33%), followed by CT (41.08%), MRI (14.22%), Mammography (7.45%), Nuclear Medicine (4.51%), and PACS (4.51%). A further 12.87% specified additional areas of work such as angiography, Cath Lab, interventional radiology, bone density and theatre imaging.
Drawing on the extensive feedback from APEX members around the country as well as data collected from Te Whatu Ora through Official Information Act (OIAs) requests and received by APEX in responses sent in June and July 2025, we have synthesised the responses of our MIT workforce with the information from the OIA to set out what we see as the problems and potential solutions to the ongoing erosion of our medical imaging services.What this report details
This report outlines what information available through the OIA and the experiences and reports of medical imaging technologists show of the situation within Te Whatu Ora’s radiology services.
To boil it down, our public radiology services and medical imaging technologists are under immense strain. This is the result of chronic understaffing, roster induced fatigue, pay disparities and outdated equipment. The pressure has got to the point where we believe Te Whatu Ora’s radiology services are unravelling.
These challenges are widespread right throughout the country. As public services become run down, they become less efficient, less safe and less attractive places to work.
In publicly owned and run radiology services, we have seen increased outsourcing of patient imaging scans to the private sector.
In just one year alone, OIA data shows this outsourcing of essential radiology services cost the public health system over $100 million. As public investment has left the public health system, large numbers of publicly trained radiology staff, both MITs and radiologists, have left work in the public health system to take up employment with private radiology services.
And as a critical mass of funding and experienced staff shifts from the public to private sector, the public sector becomes increasingly starved of the investment in radiology equipment and skilled professional labour needed to keep the system functioning. This in turn undermines the capacity of the public system to keep up with demand, leading to pressure to increase the outsourcing of medical imaging scans and reporting. This becomes a vicious cycle at the heart of the unfolding collapse within public radiology services.
Addressing these challenges is essential to ensure that New Zealanders can continue to receive safe, timely, and high-quality diagnostic imaging services within the public health system.
It is time for investment to be made. The information in this report shows that Te Whatu Ora has a clear choice.
We can either begin creating a coherent, clear plan for the rescue of our public radiology services and investing in these services. Or we can allow our public radiology services to further atrophy and unravel as exorbitant sums of public money leaves the public health system and goes to the private sector. Everything has a cost. But the information in this report shows that even with unprecedented and expensive outsourcing of medical imaging we are no closer to fixing what is becoming a broken public health system.
APEX’s Proposals to Rebuild Public Radiology Services
- End the hiring freeze for medical imaging employees, and remove the requirement radiology services receive approval of senior managers to recruit positions within services budgeted FTE;
- Develop and approve a national public radiology plan with:
- A budget for equipment purchase for end-of-life machine replacement as well as the expansion of services including into PET scanning;
- A priority list of services to which additional medical imaging FTE will be allocated and recruited to;
- Approval for currently stalled business cases made by radiology managers for equipment and workforce investment in Districts;
- Develop in conjunction with APEX new shift rosters for MITs. Beginning with the most critically fatiguing Districts, the aim would be to phase out fatiguing shift patterns and ensure better equipment utilisation including through expanding access to medical imaging through Saturdays, Sundays, and evenings.
- Recruit enough radiology assistants in each district, to support patient throughput and productivity of medical imaging services.
- Reallocate funding from outsourcing to public radiology services to run additional weekend lists to clear the growing radiology waitlists.
- Improve the salaries and working conditions of medical imaging technologists, particularly at the senior level.
- Guarantee employment for all graduates of medical imaging training programmes in New Zealand in Te Whatu Ora.
A Guide to Medical Imaging Modalities and Terms
X-Ray – A form of electromagnetic radiation that allows penetration of the human body to diagnose conditions such as bone fractures, joint problems and lung conditions such as pneumonia.
Computed Tomography (CT) – A medical imaging technique that uses X-rays and computer processing to create detailed cross-sectional images of the body. CT scan images show more detail than X-rays.
Magnetic Resonance Imaging (MRI) – A medical imaging technique which uses strong magnetic fields, magnetic field gradients and radio waves to form images of organs in the body. The scan helps doctors see soft tissues, organs, bones and other internal structures in great detail.
Mammography – A specialised medical imaging technique that uses low dose X-rays to examine the breast tissue for tumours.
Nuclear Medicine – A medical speciality that uses very small amounts of radioactive substances to produce sans and to treat diseases.
Picture archiving and communication system (PACs) – A digital system that stores, manages and distributes medical images such as X-rays, CT scans and MRIs and associated reports. MITs who work in PACS are responsible for the imaging and IT systems which radiographers and radiologists use.
Angiography – A medical imaging technique that uses X-rays to visualise blood vessels and diagnose various conditions relating to blood flow. It involves injecting a contrast dye into the bloodstream to highlights the vessels, making them visible on X-ray images.
Cath Lab – A specialised room in a hospital equipped with imaging technology for diagnosing and treating heart and blood vessel conditions.
Interventional Radiology – Medical subspeciality that uses a range of imaging technology to help guide a range of interventional medical and surgical procedures.
Bone Density – A bone density scan measures the strength of bones by measuring their density. The scan helps diagnose conditions like osteoporosis and osteopenia.
Theatre Imaging – The use of medical imaging techniques within an operating theatre during surgical procedures.
Ultrasound – A medical imaging technique which includes the use of high-frequency sound waves to create images inside of the body. The scan is useful for examining soft tissues, organs and blood flow.
PET scan – A type of nuclear medicine imaging test that uses a radioactive tracer to visualise and measure the metabolic activity of tissues and organs in the body.
MIT Staffing Pressure and Roster Fatigue — District by District
Overall Staffing Levels in Departments
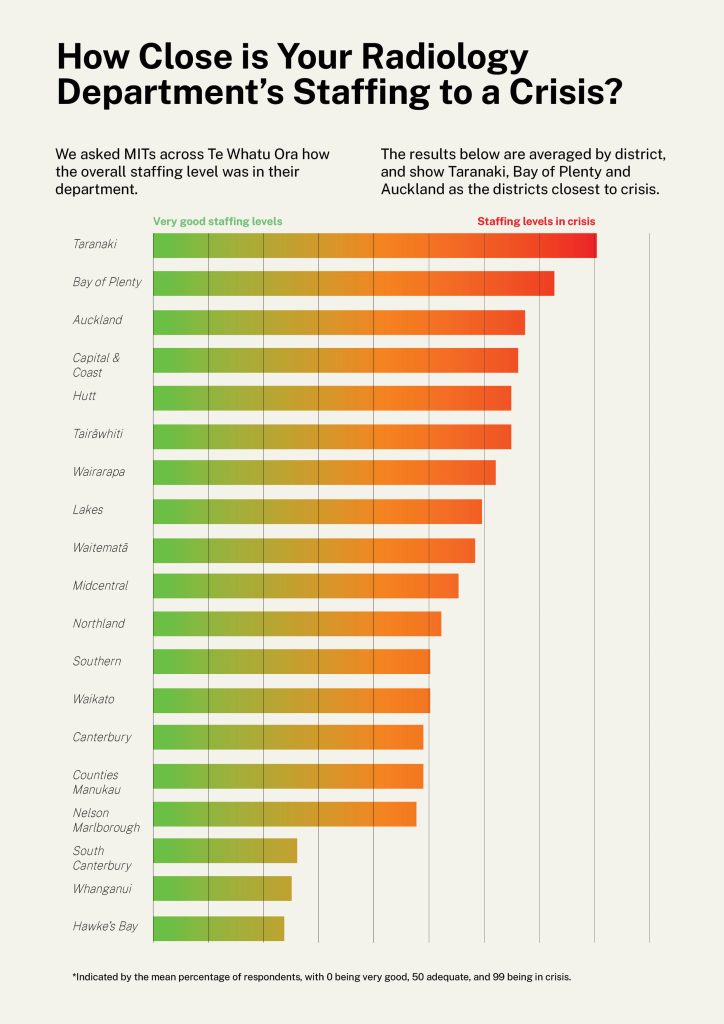
In our survey we asked MITs to rate the overall staffing situation within their departments on a 0 to 100 scale between very good levels of staffing at 0, adequate levels of staffing at 50, and crisis levels of staffing at 100.
The survey results show clearly:
- The mean overall staffing score in 11 districts was rated as inadequate.
- The overall staffing situation is rated worst by MITs in Taranaki, Bay of Plenty, Auckland and Capital and Coast Districts.
- The overall staffing situation is rated best at Hawke’s Bay, Whanganui and South Canterbury.
MIT Roster Fatigue Across Districts
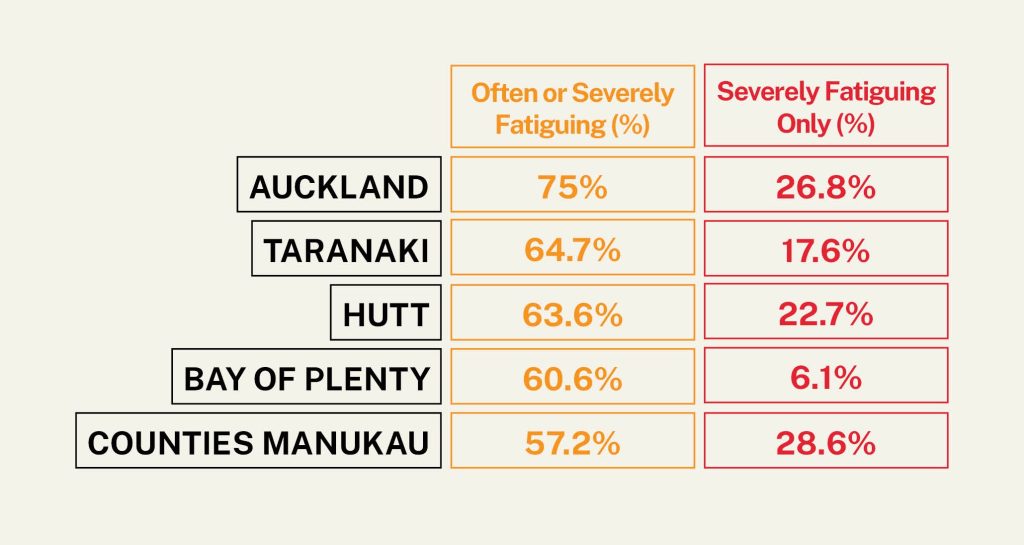
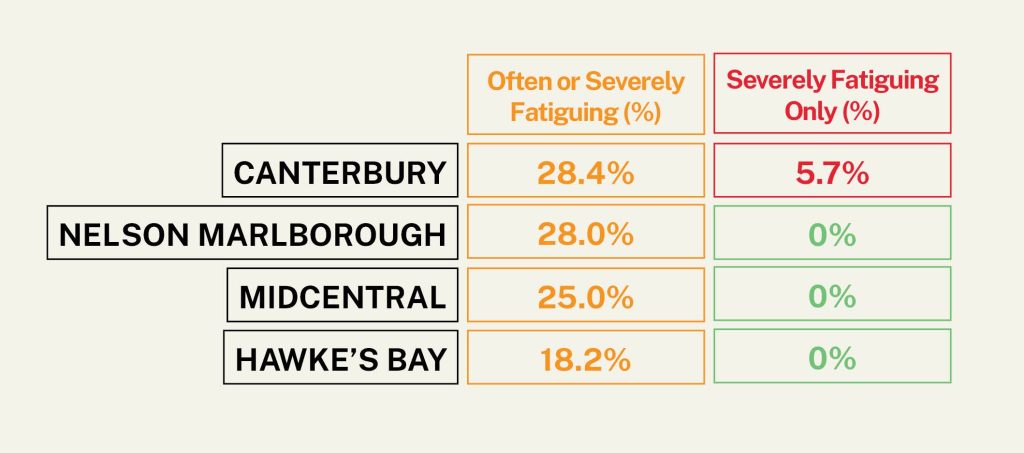
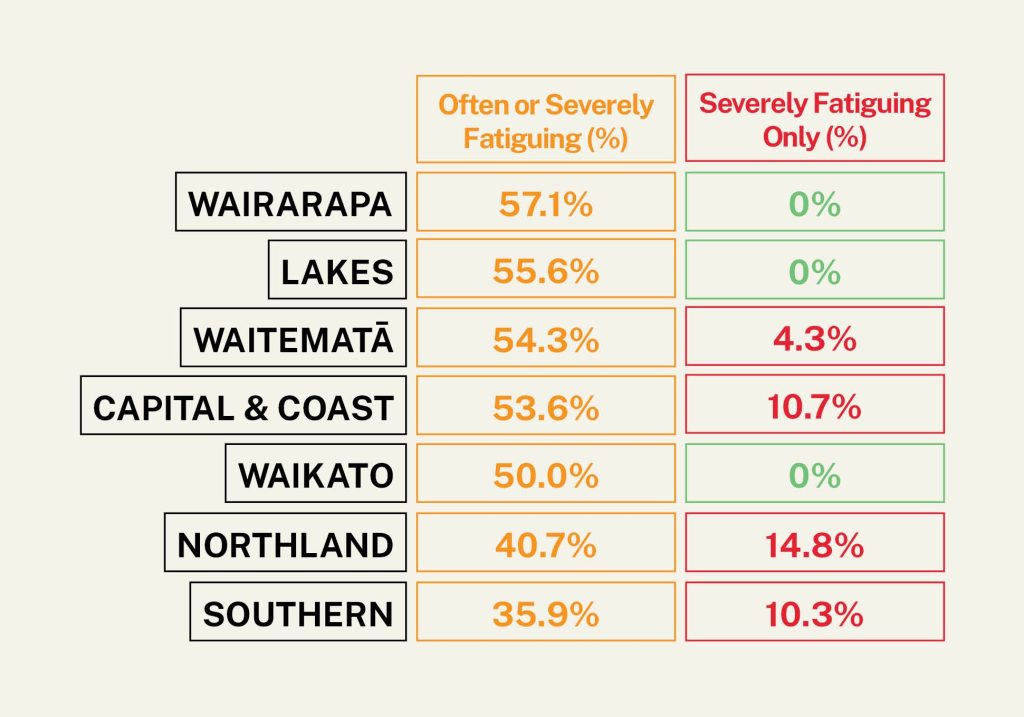
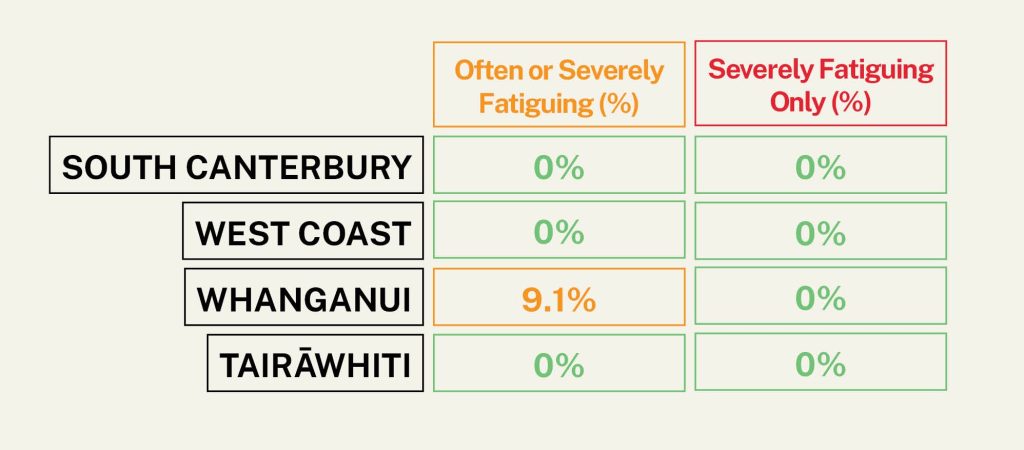
As part of our survey we asked MITs to rate how fatiguing their current rosters are. Of all respondents across Te Whatu Ora, 9.73% said their roster was severely fatiguing, 36.65% reported it was often fatiguing, *27.60% said sometimes fatiguing, 19.00% said occasionally fatiguing, and only 7.01% reported their roster was not at all fatiguing. When we analysed the responses by District, we were able to identify the Districts with the most fatiguing rosters.
Roster fatigue is a simple measure which indicates the degree to which MITs are understaffed in any department. High fatigue rosters require MITs to frequently work excessive amounts of overtime, on call and night shifts.
Most Critically Fatiguing Districts
These districts have the highest proportion of respondents reporting severe fatigue due to their rosters:
High Fatigue Districts
While not rated as “severely” fatiguing, these seven districts still show sustained pressure on staff:
Moderate Fatigue Districts
These areas report persistent but less intense fatigue levels:
Te Whatu Ora’s Vacancy Data
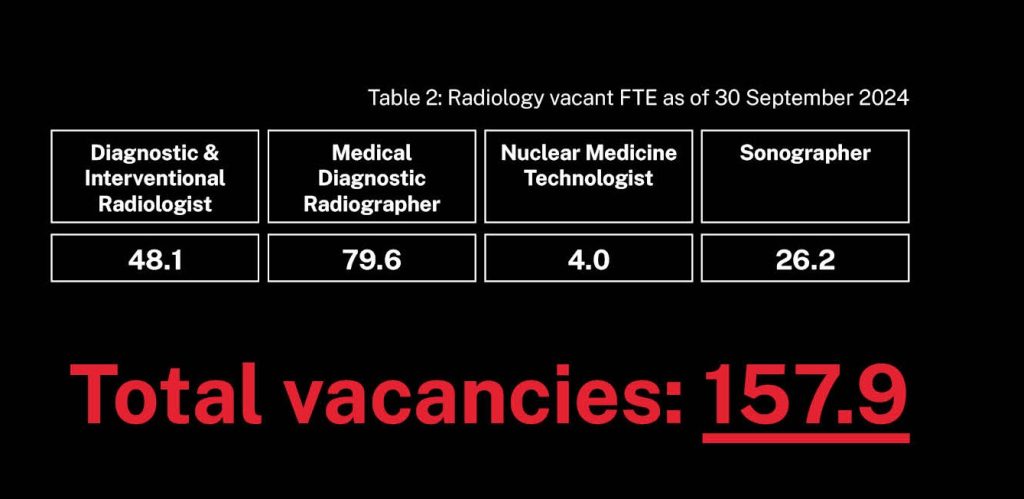
Information provided under the OIA in July 2025 from Te Whatu Ora about vacancy rates is now nearly 9 months old, and although partial and late shows that is sustained high vacancy rates within Te Whatu Ora’s radiology services. As at September 2024, Te Whatu Ora’s own data showed vacancies for 79.6 MITs, 48.1 FTE radiologists, and 26.2 sonographers.
How Understaffing Affects the Workforce
Four hundred and twenty radiographers gave written comments on the ongoing impact of unsafe staffing and fatiguing rosters on them and their colleagues.
The key impacts being experienced by respondents include fatigue and burnout, declining morale and motivation, increased sickness and sick leave, missed tea and lunch breaks and staffing/skill imbalances.
Fatigue and Burnout
Fifty-two respondents mentioned experiencing fatigue while 24 and 20 responses mentioned feeling stressed and burnt out respectively. Respondents consistently describe themselves and their colleagues as experiencing “extreme staff fatigue and burn out,” and feeling “tired and overworked at times.” This exhaustion is frequently attributed to demanding rosters and relentless workloads.
“I myself currently have a lot of 7 day runs, two days off, two days on, 7 days repeat. And it’s tiring.” – Capital and Coast
Declining Morale and Motivation
The constant pressure is contributing to a decline in staff morale and motivation. Twenty-eight responses highlighted that staff morale and motivation are being negatively affected. This widespread tiredness has direct consequences on performance, with staff also reporting decreased productivity, a decline in quality work and an increased number of mistakes.
“Poor morale, tension between management and staff due to relentless expectations of picking up shifts, tension between team members.” – Taranaki
Increased Sickness/Sick Leave
Also directly linked to the high levels of fatigue and burnout is a noticeable increase in sickness and sick leave among staff. 137 responses indicated that there are systemic issues of sickness and sick leave in their workplace, with an increase of sick days also related to mental health.
Multiple responses indicate an ongoing problem where staff burnout and sicknesses due to fatigue is high. The effects of burnout and fatigue results in increased sick and stress leave being taken, which leads to further understaffing and the cycle continues.
“People don’t hesitate to ring in sick as they can’t face another day of doing extra work due to short staffing.” – Canterbury
“When colleagues are sick, we don’t cancel patients.” – Waitematā
Break Issues
Another impact is that staff frequently experience delayed tea and lunch breaks or miss them entirely. According to 28 respondents, breaks are often postponed or skipped altogether. There is a strong consensus of there being insufficient staffing to keep up with the work, significantly disrupting break schedules.
“More pressure to add in more patients on an already stretched day… Late lunch breaks or no breaks at all.” – Capital and Coast
Staffing Imbalances
Respondents also highlighted issues with staffing imbalances. In some districts, there are critical imbalances in that services have not been reduced in correlation to having less staff which means that there is the same workload but less staff to do it. The pressure to maintain services despite shortages manifests in several ways such as forced overtime, call ins, roster instability, diversion of staff and impact on training and development.
Another issue is that even when districts appear to be “fully staffed” on paper, a large workload still falls on the shoulders of the experienced staff members, as there aren’t enough senior staff members to carry the load.
Additionally, specific modalities such as CT and MRI, are “severely understaffed,” leading to situations where trainees are left unsupported and staff members either operate beyond their scope of practice or lose out on refining their general X-ray skills.
“Staff get stuck in areas they are most needed (e.g. MRI/CT) and are losing general X-ray skills. Fatigue from on call duties.” – Lakes
“We are doing more night shifts and I have also found I’ve been working two weekends on, one weekend off more often. Everyone is starting to feel burnt out.” – Taranaki
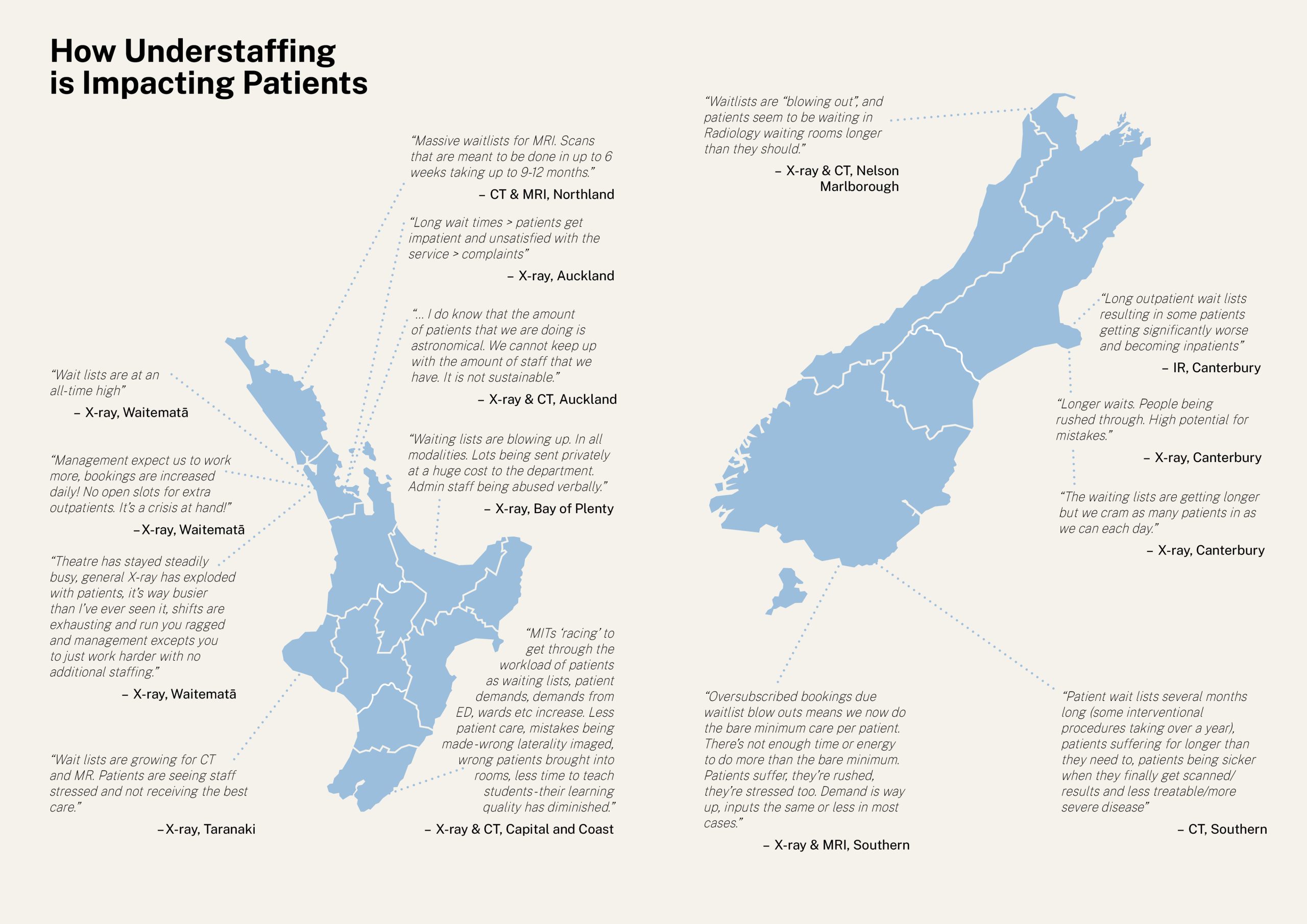
How Understaffing is Impacting Patients
MITs across Te Whatu Ora identified the ongoing staffing situation as leading to significantly increased waiting lists and times with subsequent impacts on patient care and safety.
Respondents highlighted impacts including suboptimal care for patients, delayed diagnosis and treatment, an increased risk of error, patient hostility, reduced patient-staff interaction and operational strain. Beyond initial appointment scheduling, patients also face lengthy waits in the clinic and are waiting much longer for their appointments with this extended waiting contributing to considerable patient frustration.
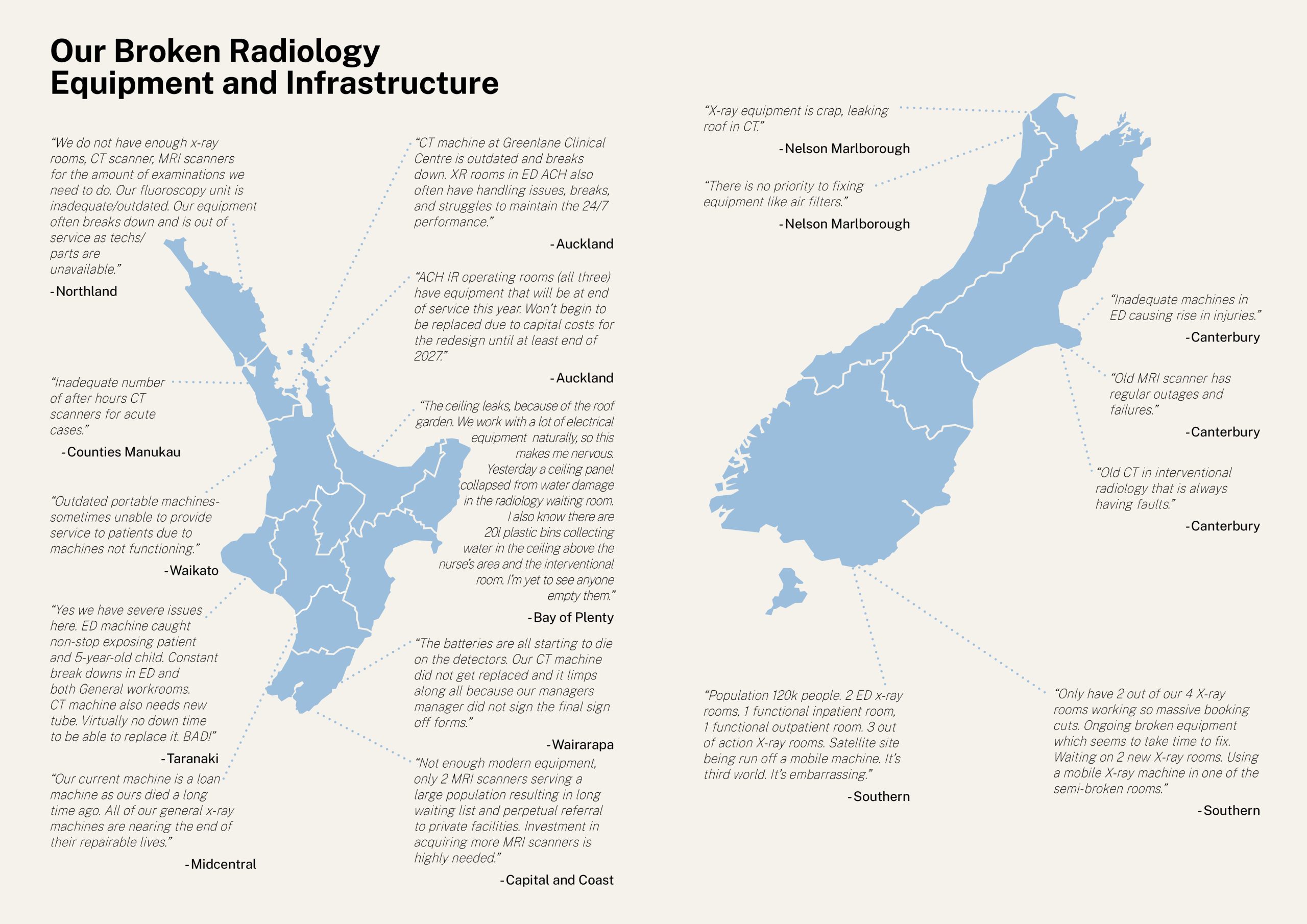
Our Broken Radiology Equipment and Infrastructure
Our survey of medical imaging technologists also identified widespread and critical equipment challenges across the radiology network.
Respondents described a system under significant strain with outdated or non-functional machines, infrastructure failures and delays in upgrades or repairs.
A recurring theme among responses was the severe shortage of functional imaging rooms and machines. Many departments are operating at half capacity or less, forcing staff to cut bookings and rely on temporary or makeshift solutions.
Equipment failures are not just an inconvenience; they pose real safety risks for both patients and staff. Multiple respondents reported hazardous situations, including malfunctioning machines and unsafe work environments.
Beyond individual equipment failures, staff identified broader systemic issues. Many departments lack sufficient imaging rooms or modern scanners to meet demand, and maintenance is hampered by unavailable parts or technicians. Staff also repeatedly expressed frustration with delayed or denied funding for essential equipment upgrades. Many believe that political and financial decisions are directly undermining patient care and staff effectiveness. The combination of outdated equipment and insufficient capacity leads to longer wait times, increased referrals to private providers and challenges in maintaining accreditation.
 44% of MITs report inadequate, broken or outdated radiology equipment.
44% of MITs report inadequate, broken or outdated radiology equipment.
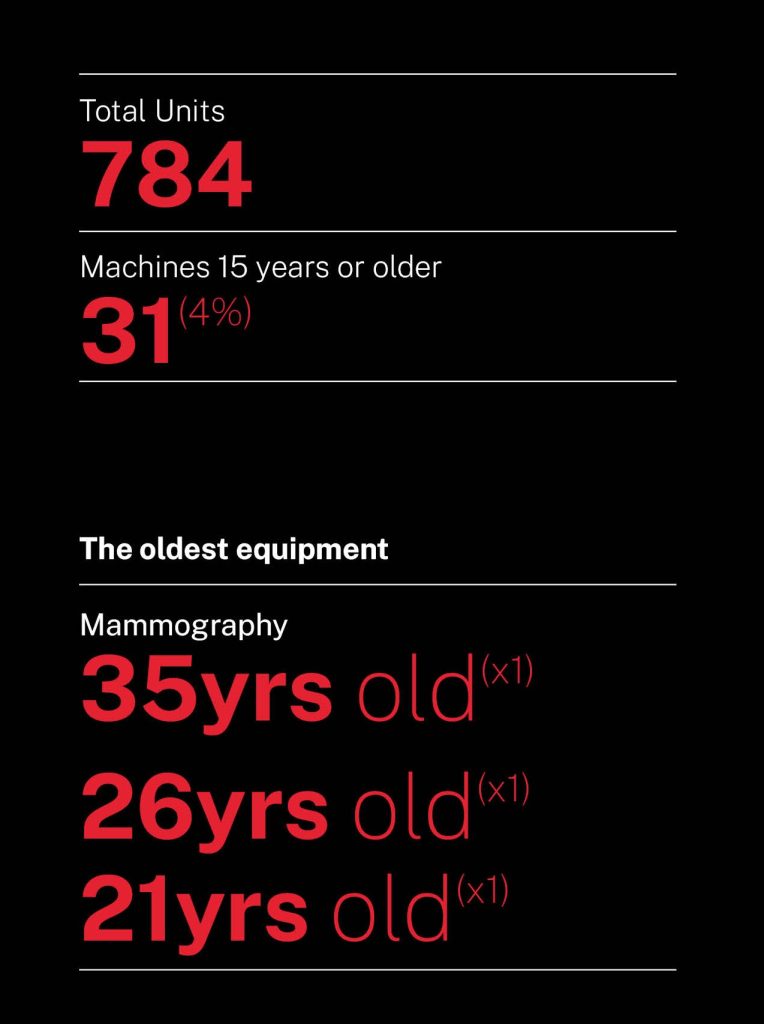
Additionally, a significant amount of equipment is outdated and in desperate need of replacement. An OIA provided dataset of nearly 800 radiology scanners reveals a concerning proportion of aging equipment, which may compromise MIT performance, diagnostic reliability and increase maintenance costs.
Out of the total 784 units, 31 machines (approximately 4.0%) are aged 15 years or older.
“The current government delayed the implementation of updating equipment in three X-ray suites.” – Northland
Outsourcing of Medical Imaging to the Private Sector
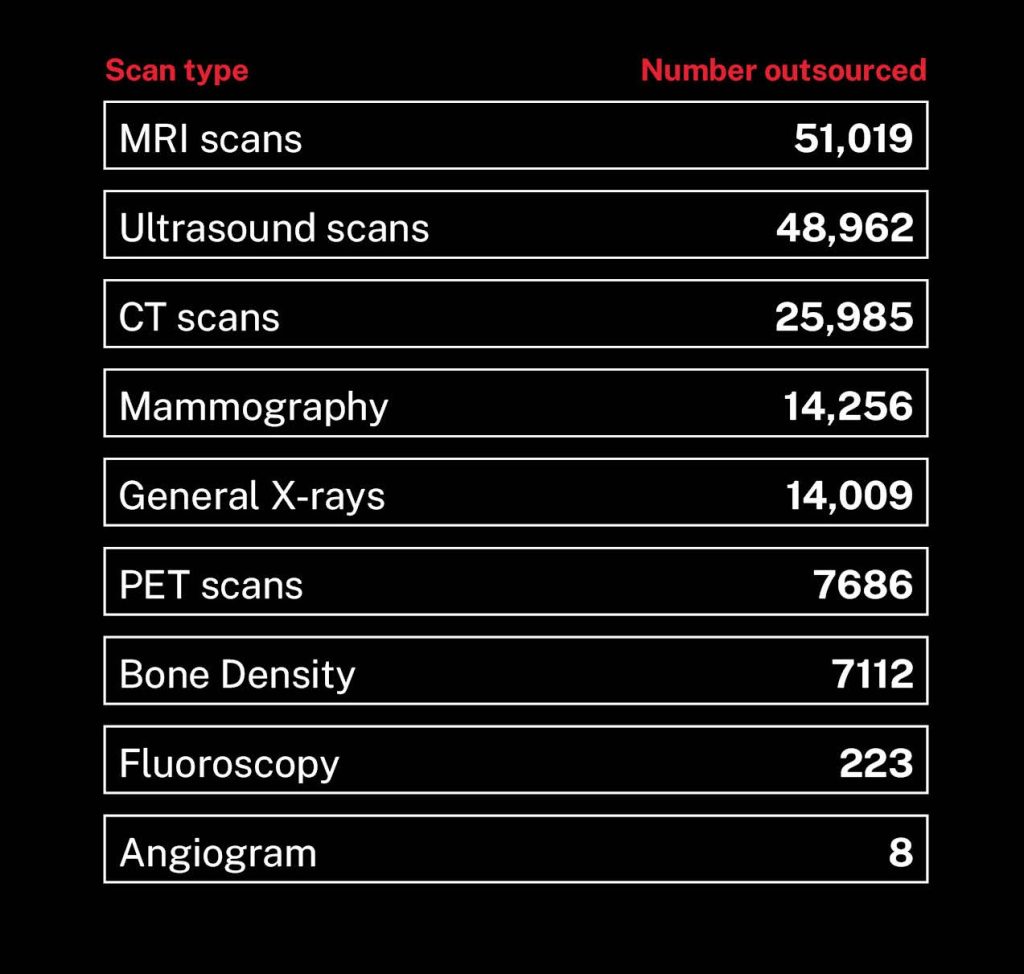
We asked Te Whatu Ora for the total number of medical imaging scans and annual spend on outsourcing by district from 1 March 2024 to 28 February 2025.
Total number and costs of outsourced scans
In the year to 1 March 2025 Te Whatu Ora outsourced over 169,276 scans (table on the right).
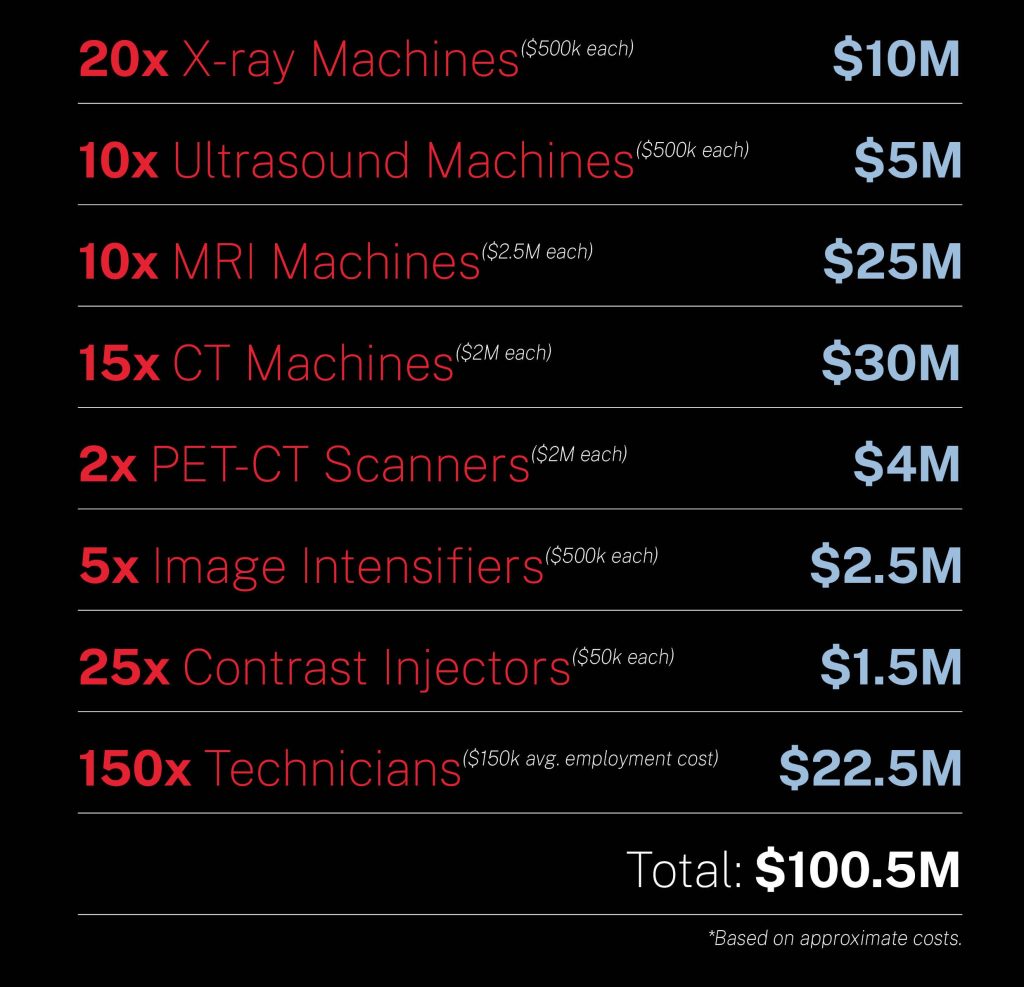
According to Te Whatu Ora, private radiology services also have ~$40 million in annual contracts for community radiology services funded through the commissioning arm of Te Whatu Ora. This means that in total over $140 million is spent by Te Whatu Ora each year on private radiology services. The costs of privatising radiology services annually is more than the total overall annual costs of the APEX MIT and MRI/NM technologist workforces which is a combined $135.2m per annum.
In one year alone, at least $100,614,789 was spent outsourcing over 169,276 scans.
.
Current Medical Imaging Waiting Lists
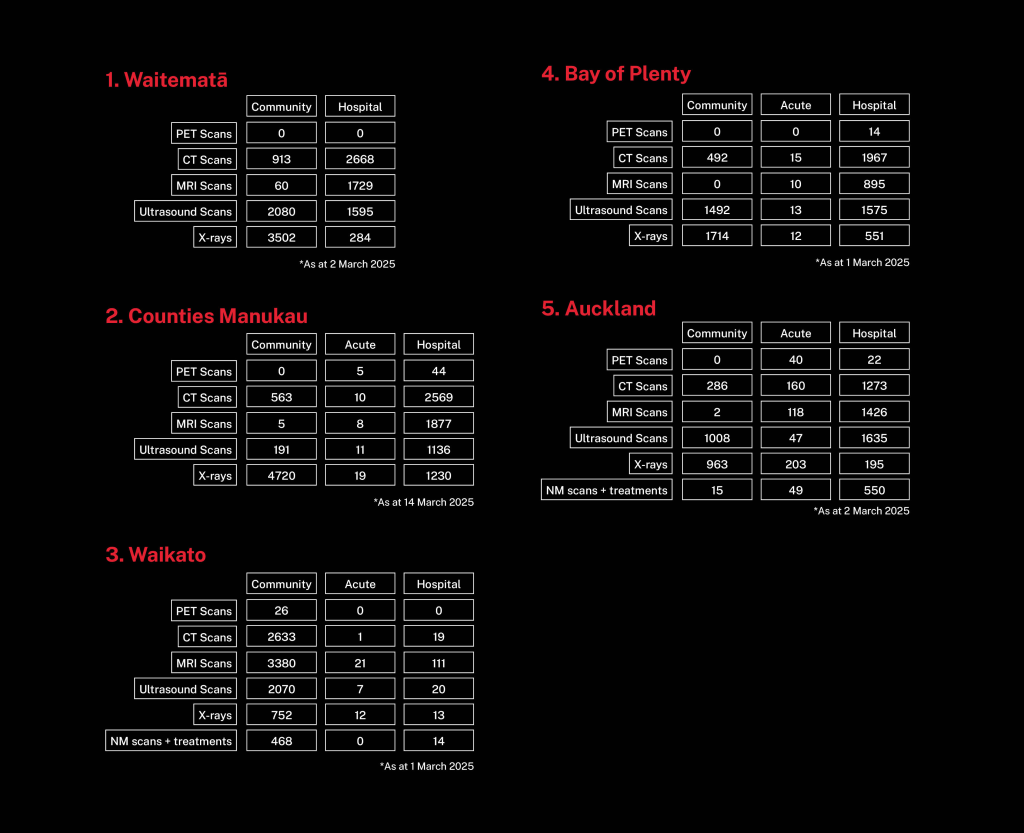
APEX requested, through the Official Information Act the number of patients as at 1 March 2025 on Districts radiology waiting lists. The waiting list information shows more than 102,446 patients waiting for medical imaging across the country and in Auckland, this includes thousands waiting for CT, MRI, ultrasound, and x-rays requested by hospital doctors.
102,446 patients are waiting for medical imaging across the country.
“Longer waiting lists tend to mean those who are quiet but in greater need are being left until last.” – Auckland
Over 50,000 patients are now waiting for medical imaging across just five districts.
Data released to us under the Official Information Act, shows that in March 2025, 50,000 patients were waiting for medical imaging. This includes thousands of urgent scans requested by hospital clinicians.
All of these districts are fast growing, upper North Island districts – Auckland, Waikato and the Bay of Plenty. Auckland’s radiology services are almost completely backlogged with over 32,000 patients wait listed.
In these districts, sustained investment to expand public radiology services is absolutely critical.
What MITs Say is Needed to Improve Radiology Services
We asked medical imaging technologists what more they would like Te Whatu Ora to do to improve our radiology services. The most common pleas were for the employer:
- Improving staffing levels, including faster replacement of staff, and increasing FTE to cover increasing workloads.
- Replacing, upgrading, or increasing radiology equipment.
- Increasing salaries and better working conditions.

 44% of MITs report inadequate, broken or outdated radiology equipment.
44% of MITs report inadequate, broken or outdated radiology equipment.